Histamine is essential to a variety of physiologic functions, and it is a versatile biologic amine involved in fine-tuning the balance between immunity and tolerance.
- Immunity is the ability to fight infection or clear abnormal cells
- Tolerance is the ability of the immune system to tolerate “outsider molecules” like foods, dust, environmental chemicals, etc.
Histamines affect dendritic cells (cells that boost the immune responses by showing antigens on their surfaces to other cells of the immune system), immunoregulatory cells, and T-cell polarization (deciding whether T-cells will have the capability to produce T1 or T2 patterns of cytokines), and cytokine production, generally. *Note: cytokine patterns:
- T1: interleukin (IL)-12 and IFN-γ
- T2: IL-4

What is the Role of Mast Cells in relation to Histamine Intolerance?
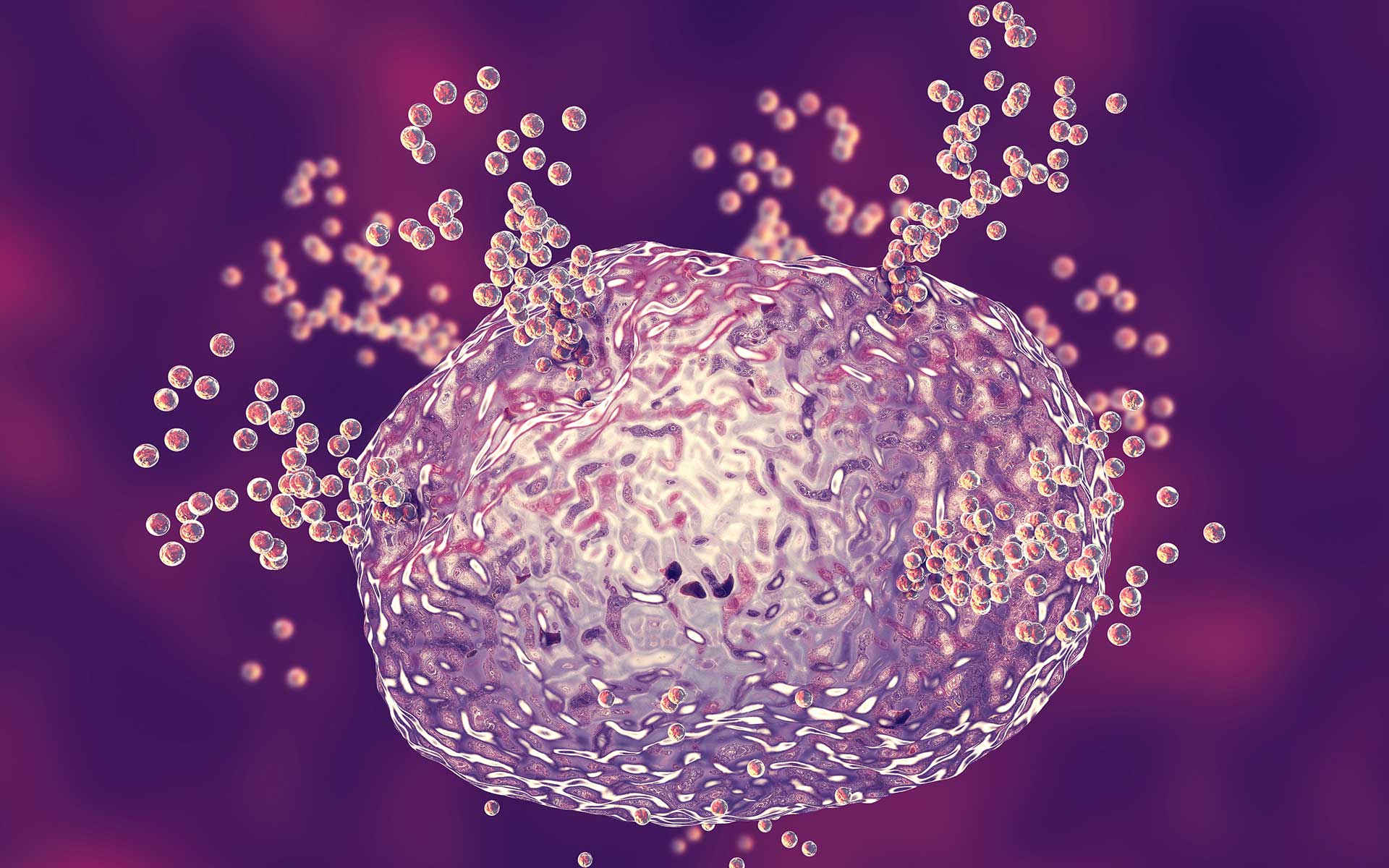
Basophils and mast cells are the most proficient histamine producers since they can store and release histamine in response to IgE-dependent or independent stimuli.
But, other immune cells, dendritic cells, neutrophils, monocytes/ macrophages, and lymphoid cells, can synthesize and release high levels of histamines under certain conditions.
Mast Cells and Immune Function in Endometriosis and Other Autoimmune Disorders
Mast Cells are activated via direct interaction with an antigen (IgE-dependent pathway stimulated by T-helper 2 (Th2) cytokines including IL-4, IL-5 and IL-13) and/or via their ability to respond rapidly to innate IgE-independent immune stimuli (IgE-independent pathway) (Binda, Donnez, & Dolmans, 2017).
In patients with endometriosis, elevated levels of IL-4 have been found in both the peritoneal fluid and the blood. IL-4 can stimulate mast cell activation, which has been associated with acute and chronic inflammation.
It is not yet known whether mast cell activation in endometriosis lesions is IgE-dependent.
Once activated, mast cells have also been found to stimulate an inflammatory reaction via the action of several mediators, including histamine proteases, and specific cytokines, such as IL-1, IL6, IL-8, granulocyte macrophage-colony stimulator factor (GM-CSF), TNF-α, and TGF-β32.
Inflammatory cytokines including IL-6, IL-8, and TNF-α have been found to be increased in the peritoneal fluid of patients with endometriosis.
Thus, histamine can be seen as a modulator of the immune response.
The activation of the immune response itself can upregulate histamine production and secretion, and the impact of the increased availability of histamine is dependent upon the receptor and cell type that it binds to.
Signs of Histamine Intolerance
First of all, histamine intolerance or sensitivity is not an “allergy” or sensitivity to histamine. It’s distinct from food sensitivity.
It’s simply excessive histamine that is trapped in the body due to too much production and release of histamine or an inability to break down the excess histamine appropriately.
It can be difficult to identify histamine intolerance because the symptoms can be vague.
Here are some signs of Histamine Intolerance to look for:
- Itchy skin, eyes, ears, and nose and/or seasonal allergies
- Dermatitis
- Chronic hives
- Burning in mouth, hands, or feet
- Swelling
- The feeling of tightness or fullness in the throat
- Flushing or temperature regulation issues
- Postural Orthostatic Hypotension Syndrome (POTS) or other forms of dysautonomia
- Dizziness, Vertigo, or even loss of consciousness
- Low blood pressure
- Tachycardia
- Heart palpitations
- Sleep disturbance
- Confusion or Irritability
- Anxiety or panic attacks
- Migraines
- Alcohol intolerance
- Caffeine intolerance
- Irregular menstrual cycle
Do you work with patients with endometriosis or other pelvic pain conditions in your practice? Interested in deeper dive training on endometriosis and pelvic pain, click here to learn more.

BECOME AN ENDOMETRIOSIS EXPERT IN 3 MONTHS!
Discover how to provide your clients with the specialized care and support to help them address their endometriosis symptoms while also growing your own practice and niche skillset.
This 3-month Certificate Program starts as soon as you enroll!
Genetics and Histamine Tolerance
Two enzymes are responsible for the breakdown and excretion of histamine when its important work as an immune modulator is done.
These enzymes are diamine oxidase (DAO) and histamine methyltransferase (HNMT).
- DAO enzyme is primarily responsible for breaking down the histamine from foods.
- HNMT enzyme is responsible for breaking down the endogenously produced histamine produced by physiologic processes.
Many people have single nucleotide polymorphisms (SNPs) in the genes that encode the enzymes. SNPs in these genes make it difficult to break down excess histamine.
For people with DAO SNPs, support with supplemental DAO digestive enzymes can be helpful.
Additionally, supplementing with riboflavin (vitamin B2), calcium, and copper supports the functioning of this enzyme.
To support HNMT SNPs, supplementing with zinc is helpful, and the ayurvedic herb salacia oblonga can regulate blood sugar and support the efficiency of the HNMT enzyme to better eliminate histamine.
Using salacia oblonga to support clients with both histamine enzyme SNPs and blood sugar dysregulation is important because metformin can further inhibit the efficiency of DAO enzyme function.
The SNP in rs1050891 of the HNMT gene can increase the risk of Parkinson’s Disease, ADHD, asthma, and migraines.
Folate, magnesium, SAMe, vitamins B1, B5, B6, and vitamin C can support the activation of the HNMT enzyme, while turmeric and caffeine, and sodium benzoate can inhibit its activity.
Nourishment to improve histamine balance
It’s important to support the body in six distinct ways if histamine intolerance is an issue for your client struggling with dysregulated immune function, such as an autoimmune disease like endometriosis, or a poor immune response to pathogens (bacteria, viruses, etc.) due to excessive inflammation.
Lower the histamine load
Add foods high in flavonoids (Fisetin, kaempferol, myricetin, quercetin, and rutin) or recommend flavonoid supplements to inhibit the release of histamine from mast cells and reduce the release of proinflammatory cytokines.
Foods high in quercetin and other flavonoids include citrus fruits, apples, onions, cabbage, cruciferous vegetables, lettuces, leafy greens, parsley, sage, and other herbs, black or green tea, and red wine.
Olive oil, buckwheat, asparagus, figs, grapes, dark cherries, blueberries, and blackberries are also high in histamine-reducing flavonoids.
Pycnogenol supplements inhibit the release of histamine from mast cells.
- Recommend that your clients eat fewer foods that are high in histamine. Don’t worry about elimination, focus on reduction and enjoyment!
- The highest histamine foods are fermented dairy products, kombucha, vegetables, pickles, cured meats, aged cheeses, alcoholic beverages, fermented soy and grains (such as sourdough bread), tomatoes, eggplant, spinach, canned fish (such as canned sardines or tuna), and vinegar.
- It’s important not to completely eliminate these foods as doing so can trigger the nervous system to develop a sensitivity to these foods. It’s better to focus on adding low histamine and high flavonoid foods vs. strictly eliminating high histamine foods.
- Notice that some of the foods that are highest in flavonoids are also high in histamine.
- It’s essential not to create fear of food within the nervous system, and instead promote the enjoyment of foods high in flavonoids.
- Even the occasional enjoyment of high histamine foods as many of these also have other benefits, such as polyphenols, probiotics, and omega-3 fatty acids. Limited consumption should be fine as long as the focus is on a whole foods diet low in packaged and processed foods.
- In fact, in the brain, histamine has a positive neurotransmitter function. It promotes motivation, supports the sleep/ wake cycle, and promotes “food anticipatory activity.”
- In other words, among the benefits of histamine activity in the brain are the enhancement of nourishing sleep, daytime motivation, and the pleasure of eating.
Eat foods high in histamine receptor antagonists
- Nettles and foods high in bromelain block the histamine receptors in allergic response symptoms.
- Drinking nettle tea, and eating pineapples and papayas, kiwi, ginger, asparagus, sauerkraut, kimchi, yogurt, and kefir support modulation of the histamine response at the receptor level.
Add DAO enzyme supplements
- Taking 1-2 capsules of DAO enzyme supplements at the beginning of each meal that contains higher histamine foods will help promote their digestion and breakdown.
Support the function of DAO and HNMT enzymes with supplemental nutrients
- Depending on your client’s specific DAO and HNMT enzyme SNPs, supplemental nutrients such as riboflavin (vitamin B2), calcium, copper, zinc, folate, magnesium, other B vitamins, and vitamin C can improve the efficiency of the enzymes that break down histamine.
- And, be mindful of excess turmeric, caffeine, or sodium benzoate in the diet depending on your client’s unique genetic risk factors.
Be mindful of probiotic supplements that contain bacteria that produce histamine
- In patients with histamine intolerance, reduced gut microbiome diversity is found.
- Additionally, patients with histamine intolerance were found to have higher levels of Proteobacteria and Bifidobacteriaceae compared with controls.
- Certain gut bacterial species have been found to secrete histamine, including Escherichia coli, Lactobacillus vaginalis, and Morganella morganii strains.
- Conversely, some species, such as Bifidobacterium longum and Lactobacillus rhamnosus have been found to reduce allergic symptoms by suppressing allergic response chemokines and downregulating mast cells.
- Plus, patients with histamine intolerance were more likely to have increased intestinal permeability (demonstrated by elevated levels of zonulin in the stool.)
Lower the load of gut irritants that can trigger a histamine response, such as yeast, dysbiotic gut bacteria, chronic infections, or parasites, and optimize digestive function.
Just like most health challenges, histamine intolerance can begin in the gut.
When clients are challenged by chronic yeast overgrowth, dysbiosis, or other chronic toxicant exposure, the immune system is chronically responsive to the irritant.
Identifying chronic and eliminating yeast overgrowth, dysbiosis, chronic infections, or other irritants, supporting detoxification pathways, and optimizing digestive function; including restoring small intestinal barrier function and healthy gut motility are key to eliminating chronic immune activation from the source.
In summary, histamine intolerance can trigger significant symptoms.
Fortunately, by reducing the histamine load, strategically antagonizing histamine receptors, and supporting optimal digestive function and a healthy, diverse gut microbiome the immune challenge of histamine intolerance that many of our clients with autoimmune diseases struggle with can be overcome.
Your clients can restore the function of the immune system and better histamine balance.
Do you work with patients with endometriosis or other pelvic pain conditions in your practice? Interested in deeper dive training on endometriosis and pelvic pain, click here to learn more.
Download your free copy of the Outsmart Endo Belly eBook!
The Professional Guide to Relieving Chronic Bloating, Pain, and Digestive Issues in People with Endometriosis

Founder & CEO
Dr. Jessica Drummond,
DCN, CNS, PT, NBC-HWC
Dr. Jessica Drummond, DCN, CNS, PT, NBC-HWC, is the founder and CEO of The Integrative Women’s Health Institute, The Outsmart Endo Health Coaching Program, and the creator of the Women’s Health Coach Certification.
She is passionate about caring for and empowering people who struggle with women’s and pelvic health concerns. She is equally passionate about educating and supporting clinicians and wellness professionals in confidently and safely using integrative tools to transform women’s and pelvic healthcare.
Dr. Drummond has two decades of clinical experience as a licensed physical therapist, licensed clinical nutritionist, and board certified health coach working with women with pelvic pain, including endometriosis, vulvodynia, and bladder pain syndrome. She brings a unique, conservative, and integrative approach to supporting women to overcome hormonal imbalances, and chronic pain conditions.
She is a sought after international speaker on topics such as integrative pelvic pain management, natural fertility options, optimal hormone health, menopause, and female athlete nutrition. Dr. Drummond was educated at the University of Virginia, Emory University, Duke Integrative Medicine, and Maryland University of Integrative Health.
Read Related Posts from The Integrative Women's Health Institute Blog: