
In a study of over 13,517 laboratory studies from 275 women, total cholesterol and low-density lipoprotein (LDl) cholesterol changes are independently affected by menopausal status and high-density lipoprotein (HDL) cholesterol is influenced by menopausal age.1
During the menopause transition, estrogen levels begin to fluctuate and eventually decline.
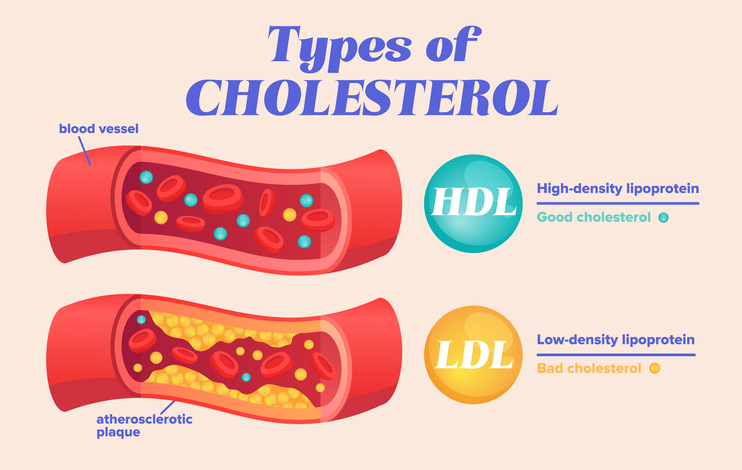
This decline can cause an increase in LDL cholesterol, also known as “bad” cholesterol. Elevated levels of LDL cholesterol are a major risk factor for heart disease.
As estrogen levels drop significantly post-menopause, heart disease risk continues to increase.
Estrogen regulates lipid balance, and thus in addition to elevated LDL cholesterol, HDL cholesterol – or “good” cholesterol – levels can decline.
Estrogen also regulates both insulin and triglyceride levels.
Triglycerides are a type of fat found in the bloodstream, and high levels can also increase the risk of heart disease.
Estrogen helps to keep triglyceride levels in check, and its decline during and after menopause can lead to an increase in triglycerides.
But why?
Download your free copy of the Outsmart Hormone Havoc eBook!
Strategies to Balance Your Hormones for Optimal Health and Weight Management
How exactly does estrogen impact lipid balance?
- Endogenous estrogens are important regulators of lipid metabolism and inhibit inflammation, vascular cell growth and plaque progression in premenopausal women.2
- Estrogen receptors are found in the liver, which is the main organ responsible for regulating lipid metabolism. When estrogen binds to these receptors, it triggers a cascade of reactions that lead to the regulation of lipid metabolism.
- The decline of estrogen levels also triggers an increase in follicle stimulating hormone (FSH) levels. Like estrogen, FSH also acts on receptors throughout the body to regulate lipid metabolism.
But, that’s not the whole story. Sometimes having elevated levels of LDL cholesterol is not dangerous.
Size matters.
Specifically, particle size matters.
When the LDL cholesterol particles in the circulation are large and fluffy, that kind of LDL cholesterol is less easily made into arterial plaque, and eventually atherosclerosis and dangerous clots. That is known as pattern A LDL cholesterol.
However, having pattern B LDL cholesterol, which is a pattern of LDL cholesterol made up of small, dense particles puts a woman at much higher risk for atherosclerosis, heart attack, or stroke.
Size also matters for HDL cholesterol. Small particle HDL is not as beneficial as larger, puffier HDL.
It’s also important to test for low density lipoprotein and intermediate density lipoprotein, which are other particles that float through the circulation and can damage the vascular epithelium (arterial walls.)
If it’s not feasible to test for particle size, The LDL/ApoB ratio is independently predictive of serious cardiovascular adverse effects in patients with established atherosclerosis.3
“If you have a fit, perimenopausal or menopausal woman, who eats a whole foods diet, exercises regularly for at least 150 minutes per week, doesn’t smoke, and has a healthy body fat percentage, she could be at low risk for a cardiovascular event, even with elevated LDL or total cholesterol.”
– Dr. Jessica Drummond
Inflammation matters too.
In the Jupiter trial4, it became clear that cholesterol is not the whole story when it comes to risk of servious, life threatening cardiovascular events.
In fact, elevated cholesterol in the context of low CRP (a measure of inflammation) was not associated with significantly increased risk of heart disease.
But, the combination of elevated LDL plus elevated hsCRP is a sign of significant risk.
Thus, if you have a fit, perimenopausal or menopausal woman, who eats a whole foods diet, exercises regularly for at least 150 minutes per week, doesn’t smoke, and has a healthy body fat percentage, she could be at low risk for a cardiovascular event, even with elevated LDL or total cholesterol.
The key is to assess her particle size and inflammatory markers, especially hsCRP.
References
- Inaraja, V., Thuissard, I., Andreu-Vazquez, C., & Jodar, E. (2020). Lipid profile changes during the menopausal transition. Menopause (New York, N.Y.), 27(7), 780–787. https://doi.org/10.1097/GME.0000000000001532
- Barton M. (2013). Cholesterol and atherosclerosis: modulation by oestrogen. Current opinion in lipidology, 24(3), 214–220. https://doi.org/10.1097/MOL.0b013e3283613a94
- DREXEL H, LARCHER B, MADER A, ET AL., – ATHEROSCLEROSIS 2021, DOI.ORG/10.1016/J.ATHEROSCLEROSIS.2021.05.010
- https://www.ahajournals.org/doi/full/10.1161/CIRCOUTCOMES.109.868299

Founder & CEO
Dr. Jessica Drummond,
DCN, CNS, PT, NBC-HWC
Dr. Jessica Drummond, DCN, CNS, PT, NBC-HWC, is the founder and CEO of The Integrative Women’s Health Institute, The Outsmart Endo Health Coaching Program, and the creator of the Women's Health Coach Certification.
She is passionate about caring for and empowering people who struggle with women’s and pelvic health concerns. She is equally passionate about educating and supporting clinicians and wellness professionals in confidently and safely using integrative tools to transform women’s and pelvic healthcare.
Dr. Drummond has two decades of clinical experience as a licensed physical therapist, licensed clinical nutritionist, and board certified health coach working with women with pelvic pain, including endometriosis, vulvodynia, and bladder pain syndrome. She brings a unique, conservative, and integrative approach to supporting women to overcome hormonal imbalances, and chronic pain conditions.
She is a sought after international speaker on topics such as integrative pelvic pain management, natural fertility options, optimal hormone health, menopause, and female athlete nutrition. Dr. Drummond was educated at the University of Virginia, Emory University, Duke Integrative Medicine, and Maryland University of Integrative Health.
Read Related Posts from The Integrative Women's Health Institute Blog:
Download your free copy of the Outsmart Hormone Havoc eBook!












