One of the most frustrating challenges that our clients with endometriosis face is how to relieve the chronic bloating known as “Endo Belly.”
Over the years, my practice has seen thousands of endometriosis warriors struggling with this, and we have developed an integrative protocol for relieving this common symptom of endometriosis, the bloat, for good.
What is “Endo Belly”?
Before we get into the steps to relieving Endo Belly, let’s talk about what it really is.
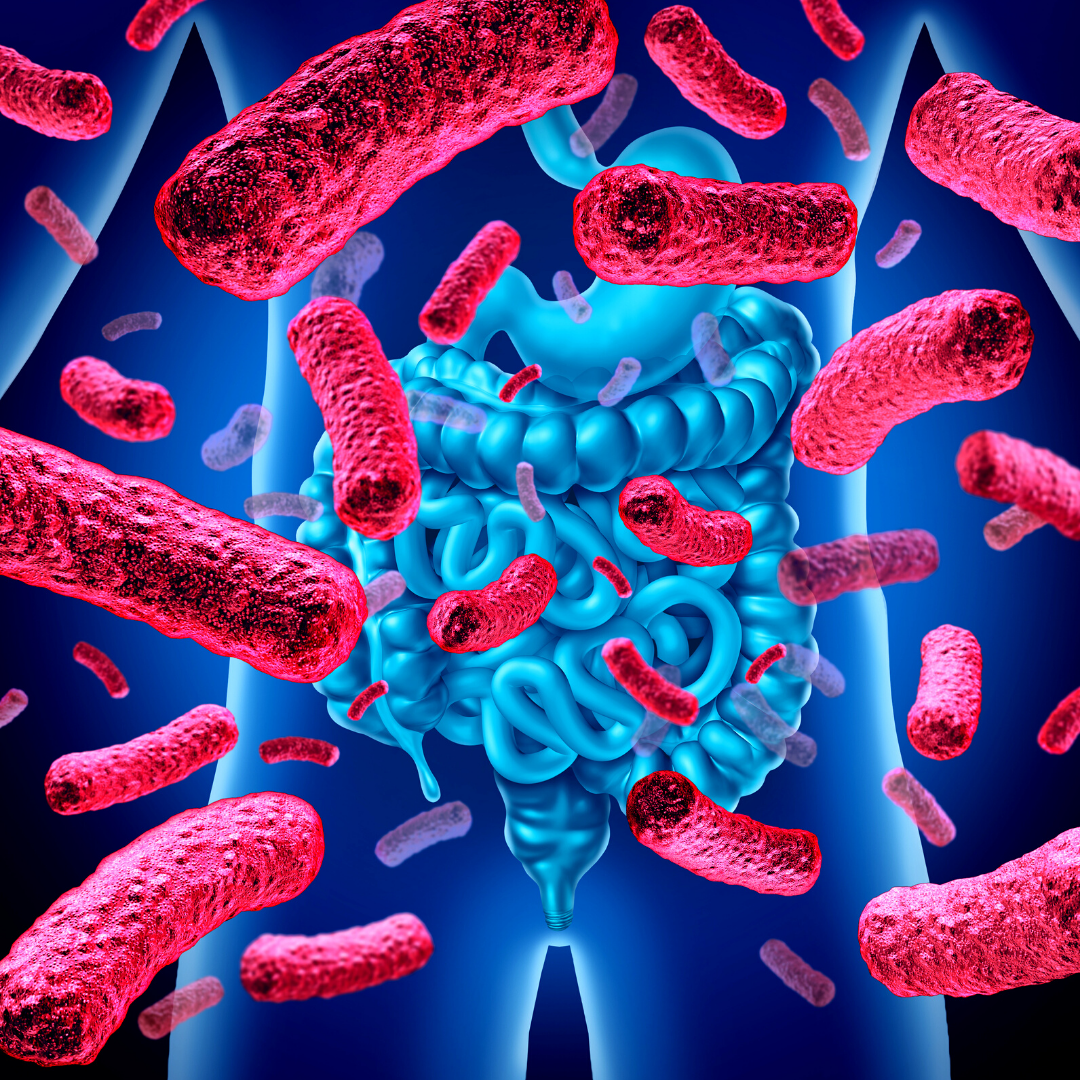
Endo Belly is the symptom of underlying dysbiosis of the small intestine and/or the colon, usually both. Dysbiosis is when the microbial community living in our intestinesgets out of balance, with the beneficial bacteria being overrun by “bad” bacteria, fungi, and other microbes.
Download your free copy of the Outsmart Endo Belly eBook!
The Professional Guide to Relieving Chronic Bloating, Pain, and Digestive Issues in People with Endometriosis
In fact, in the small intestine, the community of microbes should be quite small. When too many microbes (even some of the good guys) proliferate, bloating happens. Quite literally, the microbes in the intestines ferment the food that you eat and release gasses. It’s exactly the same thing that happens when you brew beer or kombucha.
When this happens in the small intestine, it’s called Small Intestinal Bacterial Overgrowth and/or Small Intestinal Fungal Overgrowth (SIBO or SIFO.) Associated with the microbial imbalances is inflammation, increased intestinal permeability, and stress on the immune system. (Did you know that about 80% of the immune system is in and around the digestive system?)
What is The IWHI Endo Belly/ SIBO Protocol?
Because this microbial dysbiosis is so common among our clients with endometriosis and pelvic pain, we have developed a protocol over the years to address it. We consider SIBO (or similar bacterial overgrowths or imbalances) through a wide, integrative lens to support long term healing.
One thing to keep in mind is that for people with endometriosis, the endometriosis lesions, related adhesions, inflammation, or surgeries can change the anatomy and/or motility of the intestines. When this is the case, consider that the dysbiosis will be managed over time, instead of being fully eradicated.
Enrolling now for the next session of The Outsmart Endometriosis Group Health Coaching Program. Start here today by scheduling a Strategy Session with Dr. Jessica Drummond → Click here to learn more.
How to Relieve Endo Belly Step-by-Step?
Step 1: Support parasympathetic dominance while eating. This includes strategies such as mindful eating, vagus nerve toning exercises, breathing practices, and grounding.
Step 2: Continuous improvement of heart rate variability (HRV), a measure of stress resilience. Our Outsmart Endometriosis Health Coaching programs include teaching our clients how to track their HRV using wearable technology, such as The Garmin Vivosmart Watch or Oura Ring. Understanding how eating specific foods can trigger a stress response is key to personalization of the diet, and better nutrient absorption for root cause healing.
Step 3: Enjoy delicious, pleasurable nourishment. Your “Endo Diet” should not be punishing or restrictive. In fact, most of our clients learn to expand their food choices during our program. Eating more nourishing food is key to healing.
Step 4: Finish eating for the day by 7-8pm. Eating during the most productive hours of the day is essential for blood sugar balance and hormone regulation. For many clients, changing when and how they eat is more important than changing what they eat.
Step 5: Consider the impact of surgery/ endometriosis/ adhesions/ inflammation on the anatomy and motility of the intestines. Digestive motility is key to a healthy gut microbiome, but for many people with endometriosis, digestive motility is impacted (sometimes permanently) due to the endometriosis lesions, surgeries, adhesions, and inflammation associated with the disease.
This does not mean that your digestion can’t heal, it simply means that we’ll have to take a management perspective to keep your digestion moving daily. Sometimes adding just a few simple exercises, improving your breathing pattern, or doing physical therapy or self-massage techniques is all it takes to improve the environment for a healthier gut microbiome.
Step 6: Motility support with supplementation. In addition to movement, breathing, and manual therapy practices to improve digestive motility, specific supplements can be valuable as well based on your unique presentation.
Step 7: Follow a personalized anti-inflammatory food plan. While there is no one-size-fits-all “Endo Diet,” most people will benefit from learning how to apply a personalized antiinflammatory diet in their lives based on lab and empirical testing.
Step 8: Chew each bite of food 20-40 times. (*You’ll be surprised at how much mindful eating can reduce your symptoms.)
Step 9: Utilize targeted supplementation, including digestive enzymes, betaine HCL as needed, and cycling antimicrobial herbs for at least 3 months.
Step 10: Utilize a binder such as GI Detox. While “detox” is key, elimination is even more important. You’ll learn how to support your body to eliminate well, and how to assess your daily elimination patterns.
Step 11: Use personalized supplementation and nutrition to help build up a robust, healthy colon microbiome. Using prebiotic fibers, such as onions, garlic, green banana, burdock root, green tea, FOS, psyllium, artichoke, asparagus, and targeted probiotics. Just like food, there is no perfect probiotic for people with endometriosis. We’ll test your microbiome and look for specific deficiencies or species that are overgrowing.
Why do we focus so much on the nervous system to relieve digestive bloating?
You’ll notice in the protocol above that there’s a lot of attention to calming the nervous system and optimizing stress resilience. In our practice, we track improvements in this using fitness-tracking technology.
We use many tools available for calming the nervous system to enable better digestion because after all, you can’t “rest and digest” if you’re living in “fight or flight.”
You can start today to improve your digestion by eating more mindfully, chewing 20-40 times per bite of food, adding short sessions of mindfulness or breathwork throughout the day, and eating with more pleasure.
While it’s important to have a nutrient-dense anti-inflammatory diet, how you eat is even more important than what you eat.
Enrolling now for the next session of The Outsmart Endometriosis Group Health Coaching Program. Start here today by scheduling a Strategy Session with Dr. Jessica Drummond → Click here to learn more.
How do we determine the right nutrition and supplement plan for each client?
We test and refine over at least 4-6 months. Optimizing the digestive microbiome in a world filled with stress, poor sleep, and processed foods is a challenge. Committing to the process for at least 4-6 months, and often longer, is key to taming this common symptom, Endo Belly.
During that time, we consider functional digestive testing including stool testing, gut microbiome testing, organic acids testing, genetics and epigenetics, and your body’s symptom response to dietary recommendations.
Often, your body will feel better with a committed focus on healing foods. Then, when you test foods that can cause more bloat your body will tell us if you’re resilient enough to eat them yet, or not.
The most common foods that contribute to Endo Belly are gluten, dairy, sugar, and alcohol. Sometimes raw vegetables, fruit, other grains, soy, eggs, and beans can also be contributors. But, in most cases, eventually – with proper supplementation, sleep, and stress balance – most people can tolerate all of the healthiest foods on this list.

Founder & CEO
Dr. Jessica Drummond,
DCN, CNS, PT, NBC-HWC
Dr. Jessica Drummond, DCN, CNS, PT, NBC-HWC, is the founder and CEO of The Integrative Women’s Health Institute, The Outsmart Endo Health Coaching Program, and the creator of the Women’s Health Coach Certification.
She is passionate about caring for and empowering people who struggle with women’s and pelvic health concerns. She is equally passionate about educating and supporting clinicians and wellness professionals in confidently and safely using integrative tools to transform women’s and pelvic healthcare.
Dr. Drummond has two decades of clinical experience as a licensed physical therapist, licensed clinical nutritionist, and board certified health coach working with women with pelvic pain, including endometriosis, vulvodynia, and bladder pain syndrome. She brings a unique, conservative, and integrative approach to supporting women to overcome hormonal imbalances, and chronic pain conditions.
She is a sought after international speaker on topics such as integrative pelvic pain management, natural fertility options, optimal hormone health, menopause, and female athlete nutrition. Dr. Drummond was educated at the University of Virginia, Emory University, Duke Integrative Medicine, and Maryland University of Integrative Health.
Interested in learning more about how to better support clients who are struggling with Endo Belly and associated symptoms?
Join The Advanced Women’s Health Mentorship Program for access to 35+ professional health coach trainings worth over $30,000 for one low monthly fee.
This membership includes access to our 11 pelvic pain and endometriosis related courses, including the newly updated Personalized Nutrition for Endometriosis and Pelvic Pain Masterclass ($997 value).

Read Related Posts from The Integrative Women's Health Institute Blog: